Choose the best weight loss solution for you.
Weight-loss surgery has advanced throughout its 50-plus-year history. Each of today's surgical options has unique benefits. We'll help you choose which one is right for you.
Procedure Options
Click on the different options below to learn more about each procedure we offer.
Surgical Options
The most common metabolic procedure
Often called "the gastric sleeve," the laparoscopic sleeve gastrectomy is performed by removing nearly 80% of the stomach. The remaining stomach is a tubular pouch that resembles a banana. The sleeve is an effective operation affecting the hunger and appetite centers of the brain. In other words, your body stops fighting what the brain desires.
 How the gastric sleeve works
How the gastric sleeve works
The new stomach pouch holds a considerably smaller volume than the normal stomach and helps significantly reduce the amount of food (and calories) that can be consumed. The greater impact, however, is the effect the surgery has on gut hormones that impact the body's hunger, blood sugar control and overall feeling of fullness.
The sleeve, similar to gastric bypass, is effective in terms of weight loss and improvement of type 2 diabetes independent of the weight loss.
The 'gold standard' of bariatric and metabolic surgery
The Roux-en-Y gastric bypass has stood the test of time and has been proven to be both safe and effective for most patients. Our surgical team has some of the best talent in the world, having performed this procedure for more than 20 years.
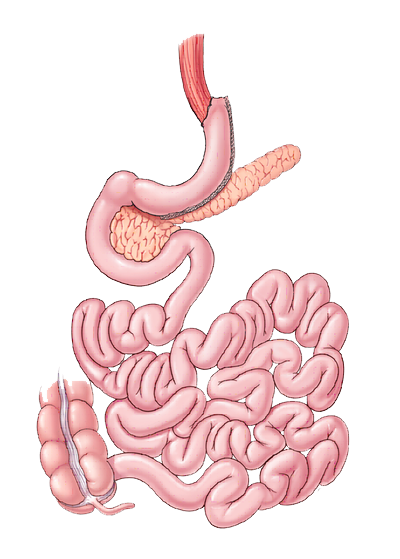
 How the Roux-en-Y works
How the Roux-en-Y works
There are two components to the procedure. First, a small stomach pouch is created by dividing the top of the stomach from the rest of the stomach. Next, the first portion of the small intestine is divided and the bottom end of the divided small intestine is brought up and connected to the newly-created small stomach pouch.
The procedure is completed by connecting the top portion of the divided small intestine to the small intestine further down so that the stomach acids and digestive enzymes from the bypassed stomach and the first portion of small intestine will eventually mix with the food.
One of the most powerful weight-loss procedures
The biliopancreatic diversion with duodenal switch (or, BPD/DS; or, duodenal switch) is considered one of the most effective operations for weight loss and metabolic syndrome, but patients may experience more frequent nutritional issues.
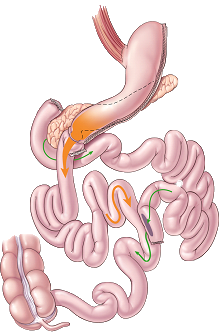 How the duodenal switch works
How the duodenal switch works
The first portion of the small intestine is divided just past the outlet of the stomach.
A segment of the last portion is then brought up and connected to the outlet of the newly-created stomach so that when the patient eats, the food goes through the newly-created tubular stomach pouch and empties directly into the last segment of the small intestine.
The bypassed small intestine is reconnected to the last portion of the small intestine so that food consumed can eventually mix with your food stream.
World-class care for all patient needs
Patients seek bariatric revision surgery for several reasons — they might not have lost as much weight as they would like to (or need to) or they might start gaining weight back again. Sometimes, revisions are needed if a patient is experiencing complications of their first operation like diarrhea, malnutrition, unexplained abdominal pain or ulcers.
With proper treatment and follow-up, however, patients can often avoid another operation. Our team is dedicated to providing world-class care for all patient needs. Very few centers have our expertise or willingness to help no matter when or where your previous surgery was done - whether an operation was done yesterday or 50 years ago, our team has the expertise and knowledge to help.
Our surgeons are well-trained in bariatric revision surgery and teach these procedures to providers all over the world. Let us help you decide if revision surgery is right for you.
Reasons you might need a revision surgery
If you're experiencing any of the following complications from your primary operation, you might need to consider undergoing a revision surgery:
Abdominal pain
Diarrhea
Inadequate weight loss
Malnutrition
Nausea or vomiting
Uncontrolled diabetes despite weight loss
Weight gain
If you believe you might need a revision surgery, contact our office at (559) 433-6010.
Endoscopic Options
Less stress. Less pain. More living.
The endoluminal gastric plication procedure (or endoscopic sleeve, or ELGP) is available to those previously denied by insurance for bariatric surgery due to low body mass index or other factors. Patients typically experience an ultra-fast recovery time (24-48 hours) and have little to no activity restrictions, once home.
How the endoscopic sleeve works
Developed in 2014, the endoscopic sleeve is an incisionless procedure that's offered to patients who aren't candidates for bariatric surgery. The procedure is completed with the use of a flexible endoscope and no incisions are made, resulting in shorter recovery time. The procedure is nonsurgical but requires general anesthesia due to the length of time to complete.
Recovery and results will vary by patient. As with any medical procedure or surgery, there are specific risks and possible complications – this may not be representative of all patients, however.
A Simple Procedure For Long-Term Weight Loss
The AspireAssist is an FDA-approved non-surgical weight loss solution affordable for patients who might not qualify for other bariatric surgeries. The 10-minute outpatient procedure is performed under general anesthesia and is reversible at any time.
How The AspireAssist Device Works
A thin tube is placed in your stomach through an endoscope and connects the inside of your stomach directly to a small button on the outside of your abdominal skin.
With the AspireAssist device, about 30% of the food that enters your stomach is removed before the calories are absorbed which results in weight loss. This emptying process is called "aspiration" and is usually performed about 20-30 minutes after you're finished eating.
The entire process takes 5-10 to complete and should be performed in the restroom so that the food that is drained can go directly into the toilet.
The different procedures will result in different degrees of weight loss,
and will have different rates of success on different diseases.
Still Have Questions? Request a Consultation
Our Team
World-Class Bariatric
& Metabolic Surgeons
& Metabolic Surgeons
Our staff is here to help you make the best decision for your needs and will be with you every step of your surgical journey.
Leadership
Program Director
Dr. Kelvin Higa
Dr. Kelvin Higa
Dr. Kelvin Higa, former President of the American Society for Metabolic and Bariatric Surgery (ASMBS) and the International Federation for Surgical Obesity and Metabolic Disorders (IFSO).